Connect With Us
Blog

Managing Toenail Fungus Infections

Fungal toenail infections, or onychomycosis, account for approximately 50 percent of all nail diseases, particularly affecting toenails. Laboratory diagnosis through microscopy and culture of nail clippings is recommended before starting treatment to confirm the infection type. For patients requiring treatment of fungal toenails, oral antifungal medications are typically used for severe infections, while topical antifungals are suitable for superficial or minor cases and for those unable to take oral medications. The duration of treatment varies, with systemic medications typically requiring a few months and topical treatments possibly extending up to two years. Patients should be aware that treatment success rates vary, and nails may not return to a completely normal appearance even after successful therapy. Additionally, there is a risk of treatment failure or relapse, necessitating further diagnosis and possibly alternative treatment strategies. Ultimately, the decision to treat fungal nails should be individualized, considering the patient's overall health, risk factors such as diabetes or vascular disease, and the severity of the infection. If you have developed a fungal toenail infection, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment suggestions.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Howard Kimmel, DPM of Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Uncomfortable Foot Pain
 Feet endure a lot of stress, carrying our body weight over countless miles throughout a lifetime. This constant use can lead to various sources of foot pain, making even basic activities like walking painful. A common cause of foot pain includes plantar fasciitis, characterized by sharp heel pain due to inflammation of the tissue connecting the heel to the toes. Bunions, which are bony bumps forming at the base of the big toe, can also cause significant discomfort. Flat feet, where the arches collapse, can lead to pain and fatigue in the feet and legs. Additionally, arthritis can affect the joints in the feet, leading to chronic pain and stiffness. Treatments for foot pain vary depending on the cause but often include rest, compression, and elevation. Orthotic inserts and wearing proper footwear can also provide relief. In more severe cases, medical interventions such as corticosteroid injections or surgery may be necessary. If you are experiencing persistent foot pain, it is suggested that you see a podiatrist for a proper diagnosis and a tailored treatment plan.
Feet endure a lot of stress, carrying our body weight over countless miles throughout a lifetime. This constant use can lead to various sources of foot pain, making even basic activities like walking painful. A common cause of foot pain includes plantar fasciitis, characterized by sharp heel pain due to inflammation of the tissue connecting the heel to the toes. Bunions, which are bony bumps forming at the base of the big toe, can also cause significant discomfort. Flat feet, where the arches collapse, can lead to pain and fatigue in the feet and legs. Additionally, arthritis can affect the joints in the feet, leading to chronic pain and stiffness. Treatments for foot pain vary depending on the cause but often include rest, compression, and elevation. Orthotic inserts and wearing proper footwear can also provide relief. In more severe cases, medical interventions such as corticosteroid injections or surgery may be necessary. If you are experiencing persistent foot pain, it is suggested that you see a podiatrist for a proper diagnosis and a tailored treatment plan.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Howard Kimmel, DPM from Buckeye Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Cracked Heels and Running

Cracked heels, a common foot ailment, can occur both before and after running, presenting discomfort and aesthetic concerns. Before running, dry skin and lack of moisture contribute to heel fissures, exacerbated by friction and pressure during physical activity. These cracks can deepen and worsen post-run due to prolonged pressure and sweat accumulation, leading to pain and potential infection. Prevention is key in addressing this issue. Regular moisturization, particularly before running, helps keep the skin supple and prevents excessive drying. Wearing properly cushioned and supportive footwear, as well as moisture-wicking socks, reduces friction and minimizes the risk of developing cracks during exercise. After running, it is important to clean and dry the feet thoroughly, applying moisturizer to soothe and hydrate the skin. Additionally, addressing any existing cracks promptly with foot creams or ointments helps expedite healing and prevents further complications. If you enjoy running and have developed cracked heels, it is suggested that you speak with a podiatrist who can offer you effective prevention and treatment techniques.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Howard Kimmel, DPM from Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Can Bunions Become Worse?

A bunion, medically termed hallux valgus, is a bony bump that forms at the base of the big toe. This condition develops when the big toe pushes against the adjacent toe, causing the joint to protrude outward. Bunions can result from various factors, including genetics, wearing tight or ill-fitting shoes, and foot injuries. Individuals with certain foot types, such as flat feet or low arches, are more prone to developing bunions. Additionally, occupations or activities that involve repetitive stress on the feet can increase the risk. Bunions are a relatively common foot ailment, affecting millions of people worldwide, with women being more susceptible than men as a result of wearing high heels or narrow shoes that can worsen the condition. While bunions may initially cause mild discomfort, they can progressively worsen, leading to pain, inflammation, and difficulty walking. A bunion can be uncomfortable, and a podiatrist can offer you effective relief strategies. If you have this condition, it is suggested that you consult this type of doctor who can offer appropriate treatment methods.
If you are suffering from bunion pain, contact Howard Kimmel, DPM of Buckeye Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
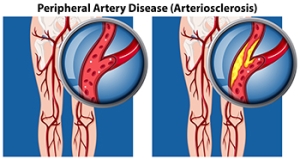
Causes and Diagnosis of Peripheral Artery Disease
Peripheral artery disease, or PAD, poses significant challenges for foot health, stemming from restricted blood flow to the lower extremities. This condition, often caused by atherosclerosis, involves the buildup of fatty deposits in the arteries, leading to narrowed or blocked blood vessels. The diminished blood supply to the feet can result in various symptoms, including pain, cramping, numbness, and weakness, particularly during physical activity. Left untreated, PAD can contribute to serious complications such as foot ulcers, infections, and delayed wound healing. Diagnosing PAD typically involves a comprehensive evaluation by a podiatrist. This process includes a thorough medical history review, assessment of risk factors such as smoking and diabetes, and a physical examination focused on evaluating circulation in the legs and feet. Specialized diagnostic tests, such as ankle-brachial index, or ABI measurement, Doppler ultrasound, and angiography, may also be employed to confirm the diagnosis and determine the extent of arterial blockages. If you are experiencing any of the foot symptoms mentioned above, it is suggested that you consult a podiatrist who can accurately diagnose and offer relief solutions for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Howard Kimmel, DPM from Buckeye Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Brook Park and Willoughby, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.